Spirituality is considered a social determinant of health that is linked to human goods and integrating spiritual factors into public health and medicine are being adopted in current practice in the United States (Long, Symons, et al., 2024). This study provides evidence-based recommendations derived from a national multidisciplinary Delphi panel that reviewed 586 studies addressing spirituality in serious illness and health. The generated evidence-based included: 1) recognize spirituality as a social factor associated with health in research, 2) community assessments, and program implementation; 3) incorporate person-centered evidence-based approached of spiritual community participation to improve medical care and population health; 4) educate public health professionals and medical providers about empirical evidence related to spirituality and health; and 5) provide spiritual care and support within health systems through chaplains and other specialist (Long, Symons, et al., 2024).
Social determinants of health (SDOH) are social and environment factors that affect an individual or entire community’s health status (Pinals et al., 2021). Pinal et al. (2021), suggested that social determinants of mental health are nuanced factors that influence an individual’s emotional and psychiatric well-being. This study was informed by the following overarching question: How can integrating spiritual care improve mental health with proper treatment and spiritual public health?
Long, Symons, et al. (2024) reported that spiritual needs of patients remain under addressed in clinical settings. According to these same authors, validated tools such as the FICA (F: faith, belief, meaning; I: importance and influence; C: community; A: address or action in care) spiritual assessment tool, can enhance whole-person care by identifying which patients might benefit from spiritual support or spiritual community participation.
Wiggins (2018) discussed the past and recent research on spiritual care integration within mental health. Wiggins reviewed Fallot’s concepts of how spirituality plays a positive role in religious coping. Fallot suggested prayers helps to avoid negative activities such as drug use. In the reviewed studies, religious coping helps with decision-making, is highly associated among patients with fewer depressive symptoms, and improves the quality of life.
Wedgeworth (2023), uses the SDOH model to explain how living conditions affect the development of health conditions. The SDOH model consists of five domains: 1) economic instability, 2) education access and quality 3) healthcare access and quality 4) neighborhood and built environment and 5) social and community context. The same author suggests spirituality should be added to this model and nurses should incorporate spiritual assessments into holistic patient care. This may bring about better physical, psychological and quality of life outcomes.
Jastrzebski (2024) suggests there are links between religious behavior and social health through activities such as, religious service attendance or meetings with clergy, and found that attendance at religious services was related to longer life expectancy. Spirituality has influence on human health in three distinct waves: a general relationship between religion or spirituality and health often focuses on the frequency of prayer and attendance at church, the unique effects of spirituality on health and the casual role of spirituality on mental health as well the meditating role of spirituality in a clinical setting.
Koenig (2017) highlighted the Screening Spiritual History (SSH) assessment which provided the following question as an example for a clinician to ask their patients. How important is religion in your daily life? Koenig argued understanding the religious background of the patient can help explain the patient’s attitudes on a wide range of issues. For example, knowing a patient’s faith denomination can assist the therapist to determine a therapeutic approach. In addition, a Christian may enjoy prayer and exercise as a part of treatment (Koenig et al., 2017).
In recent years, health care systems are focusing more on social determinants of health, attending to community and spiritual health is becoming a priority for spiritual care providers. Chaplains can rely on existing models of faith-health partnerships to improve health (Fleenor, 2021). Researchers have begun to investigate the differences between quality improvement and evidence-based practice in spiritual care. Monet (2017) examined evidence-based practices in spiritual care consisting of clinicians and chaplains. Both chaplains and clinicians expressed interest in assessing patients’ culture, psycho-spiritual, well-being, trust-building and meaning in life (Monet, 2017). In addition, the study showed assessments can show patient’s beliefs and faith background.
Vieten et al. (2023) reported 89% of mental health professionals agreed that clinicians should receive training in Religion and Spirituality (R/S) competencies. In addition, studies report there are currently no formal assessment or treatment guidelines for psychiatric clinicians to address Social Determinants of Mental Health (SDoMH) (Jeste et al., 2025). SDoMH are factors such as childhood abuse and neglect, trauma, violence, discrimination due to stigma, social isolation, unemployment, food insecurity, housing instability and incarceration that can influence treatment of mental disorders (Jeste et al., 2025). Long, Rosmarin, et al. (2024) reports the state of California is now exploring how Medicaid funds can help faith communities and ministerial associations address health-related social needs within congregational settings.
Core Definitions of Spirituality and Religion
According to research, multidisciplinary international consensus conferences defined spirituality as a "dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence, and experience relationship to self, family, others community, society, nature, and the significant or sacred, and religion as the search for significance within the context of established institutions oriented to facilitating spirituality (Long, Symons, et al., 2024).
Cultural Competency
When patient’s religious and health care needs are met culturally, this can help improve their quality of care. Swihart (2023) defined cultural competency as the ability of health providers and organizations to deliver health care services that meet the cultural, social, and religious needs of patients and their families. Providing culturally competent health care training is needed for clinicians to provide culture-specific values in health promotion and cultural awareness training (Swihart et al., 2023).
According to Long, Symons, et al. (2024) the role of training in organizational development and concluded training sessions should include employee empowerment skills, conflict management, and the practice of forgiveness, acceptance, and gratitude. Healthcare professionals do not always feel comfortable addressing the spiritual needs of their patients. Therefore, the role of training in organizations may empower healthcare professionals. Training can help them to develop spiritual care skills which will benefit their patients (Morrison & Furlong, 2019).
Puchalski and Sbrana (2019) reported that 45% of healthcare professionals felt they were able to address their patients’ spiritual needs, and many reported a lack of education and training. Examples to integrate spiritual values into healthcare are as follows: make an empathic connection between the clinician and patient, discuss values, beliefs, and what matters most to the patient, discuss clinical data and diagnosis, and decide together what is the best treatment for the patient (Puchalski et al., 2019).
Effectiveness of Spiritual Assessments
The effectiveness of spiritual care assessments indicate clinicians will begin to become sensitive to patients as they share their intimate thoughts about their spiritual values. In addition, clinicians will develop a partnership with the patient, which will help make a better diagnosis and effective treatment plan. The patient will gain insight into self-awareness, decision-making, and action planning. In addition, “The choices the counselor makes during the initial assessment phase of counseling can influence the client’s level of safety with disclosure and the counselor’s level of accuracy and completeness of client conceptualization” (Cashwell & Young, 2014). The assessment provides benefits for both clinician and patient along with effective treatment plans.
Puchalski and Sbrana (2019) suggested spiritual history tools used such as Faith, Importance/Influence, Community, Action/Address in care or FICA. The FICA tool identifies spiritual strengths and distress. The tool also assesses the patient’s faith, belief, meaning, and importance of spirituality in their life. In the reviewed studies of spiritual screening, obtaining
spiritual distress and issues during follow-up visits allow clinicians to find out if there is: a change in clinical status, increased pain, or distress, and unclear aetiologies for patients with concerns to evaluate for all aetiologies including spiritual. In addition, spiritual distress consists of existential distress, hopelessness, despair, and anger at God (Puchalski et al., 2019).
Religious Coping in Mental Health
Jastrzębski (2024) addressed how religion and spirituality is helpful in overcoming emotional distress and a representative sample of the global community revealed that religious involvement such as frequent church attendance averts or decreases depressive disorders.
Studies show the Religious Coping Theory (RCT) has five domains: discover meaning, gather control, find closeness to God, find closeness with others, and transform lives. People who suffer from mental illness find solace within their congregation and community (Xu, 2016). RCT is very important and helpful for chaplains and clinicians to understand how to diagnose their patients’ spiritual concerns. RCT can be beneficial for both patients and healthcare professionals.
Religious Coping Styles
Jianbin Xu (2016) examined Kenneth Pargament’s three coping styles: self-directing, deferring, and collaborative. During the self-directing style, the individual problem solves on their own. In the deferring style, the individual depends on God to problem solve for them.
During the collaborative style, both individuals and God work together to resolve problems. Xu suggests these coping styles treat the whole person and falls in line with holistic care.
Social Determinants of Health &Theoretical Framework
Spiritual leaders such as chaplains within healthcare organizations and military were interviewed to find out about their views and concepts on mental health in the community. In addition, mental health clinicians, were interviewed and surveyed to share their views on how they incorporate spiritual care within mental health treatment to help patients who struggle with mental illness. The theoretical framework for the study was centered around spiritual assessment tools such as the FICA assessment to see if participants were assessing patients’ spiritual care. It also focused on the training and education of chaplains and clinicians.
Spiritual care has re-emerged and is becoming an important discussion in mental health and human services. According to Regis (2025) human service organizations can integrate spiritual care into their social work programs to support individuals’ overall well-being. This article suggests incorporating spirituality into social work will help clients explore their spiritual aspect of their lives. It also states, social workers do not feel prepared to initiate or participate in spiritual discussions due to lack of training on the topic. Courses on spirituality and social work are recommended in providing care and furthering the profession (Spirituality in Social Work: Improving Patient Care, 2025).
Lee (2025) suggests spiritual care is an essential component of community health and can be integrated into human services programs. Spiritual care provides emotional support during times of crisis, fosters a sense of community and social connection, promotes healthy behavior and lifestyle choices and enhances overall well-being and quality of life. Examples of spiritual care programs implemented in public health settings include: 1) The Centering Prayer Program, 2) The Faith Community Nursing Program and 3) The Spiritual Care in Palliative Care Program (Lee, 2025).
Current State of Spiritual Care Practice and Mental Health
Fleenor (2021) suggest chaplains should look to existing models of faith-health partnerships that bring together communities of faith and health care systems to improve health. He further states, chaplains have neglected large-scale population level initiatives but instead should focus more on social determinant of health to improve public spiritual health.
Literature Review Summary
Much of the literature on spiritual care indicates spiritual care can provide hope and motivation for people who suffer from mental illness. Integrating spiritual care will improve mental health treatment within the mental health industry. In doing so, clinicians must learn and request more spiritual resources or definitions. More clinical spiritual assessments need to be conducted on mental health patients. More collaborations are needed with the clergy community and clinicians. In addition, better clinical training in religion and spirituality is needed for mental health clinicians.
In the reviewed studies, research found clinicians should have more discussions and lectures on religion and spirituality during their graduate-level courses. Mental health providers will feel more comfortable with referring patients to clergy and conducting spiritual assessments once they have had proper training and education. Studies also indicate that there is an elevated level of church attendance among those who suffer from mental illness. Many rely on their faith and religion to help cope with depression and anxiety. Spiritual care integration can change lives and bring about lifestyle transformation.
The studies in this review of spiritual care found spirituality is considered a social determinant of health. Long, Symons, et al. (2024) reports validated tools such as the FICA may help address gaps of under addressed spiritual needs of patients. Patients who were assessed with tools had fewer depressive symptoms, better quality of life, and a stronger rapport with physicians. Some scholars reported the integration of spirituality and health represent “FaithHealth,” system to strengthen population health.
Research Questions
This study had four overarching research questions:
-
How can integrating spiritual care improve mental health with proper treatment and spiritual public health?
-
Do mental health clinicians use spiritual care assessments and are they trained in spiritual care, and if so, how?
-
Do mental health clinicians collaborate with clergy, and if so, how?
-
What barriers do mental health clinicians face in integrating spiritual tools into mental health treatment?
Methodology
Research Design
The research design consisted of qualitative research with survey data collected via Survey Monkey and telephone interviews conducted with a sample of chaplains and clinicians to obtain their personal view about using spiritual care tools and integrating spiritual care within mental health therapy. The study sought to identify whether clinicians used spiritual care assessments with their patients and barriers in using spiritual care assessments and spiritual care within mental health treatment.
The research design has several sources of evidence indicating it is a valid research process from similar studies. For example, Addressing Religion and Spirituality in the intensive care unit: A survey of clinicians. Choi et al. (2019) surveyed 219 ICU clinicians to see how they address religious and spiritual needs of patients. Results showed most clinicians agreed it is their responsibility to address religious and spiritual needs of patients. The study reported clinicians felt comfortable speaking with patients about their spiritual concerns.
The study Integrating Spiritual Care Within Mental Health’s survey and interview questions identified if clinicians and chaplains need further training in spiritual care, chaplains and clinicians reported on their experiences, client outcomes, and treatments. The principal investigator (PI) tailored the phone interview questions from a study by Fang et al. (2022) suggests the reliability and validity of Results by Unit on The Spiritual Care Competence Scale (SCCS) were demonstrated. The study explored whether nurses were trained to assess patients’ spirituality and design and implement a plan of spiritual care.
Target Population and Participation Selection
Interviews were conducted with chaplains within healthcare organizations and military. Mental health clinicians were interviewed by various cities. Advent Health University (2021) states the role of chaplain provides spiritual care for individuals in non-religious organizations (Chaplain vs. Pastor: What’s the Difference, 2021). According to Law Insider (2022), mental health clinician definition means a licensed treatment provider as a psychiatrist, psychologist, clinical social worker, or counselor permitted to evaluate and care for the mental health needs of an individual (Mental Health Clinician Definition, 2022).
Participants consisted of a convenient sample of five chaplains and five clinicians recruited by PI’s existing personal/professional network, through snowballing or chain recruitment strategy. The PI chose snowballing or chain recruitment to help reach chaplain and clinician population from existing personal/professional network.
Participants
A checklist of chaplains and clinicians were gathered. The PI interviewed participants by telephone and submitted a survey along with a consent form. The PI contacted chaplains and clinicians to set up appointments by phone and email. The PI utilized email to forward a survey link to chaplains and clinicians. The following steps were done to obtain site permission, email clinicians’ an invitation with surveys/consents, obtain clinician’s/chaplain’s emails, and follow-up phone interviews. Ten participants completed their study.
Participant Demographics
The participants were from the following states Arkansas, Georgia, Tennessee, Texas, Alabama, and Utah. The PI selected those states because professional existing personal/professional networks facilitated those connections.
Measures
The Survey Monkey data was used to identify if clinicians understood the importance of assessing patients’ faith background, and any existing barriers, and to encourage clinicians to use spiritual care tools for patients with unmet spiritual needs. The clinicians and chaplains were asked five questions regarding their knowledge of spirituality, spiritual well-being and how patients respond to spiritual assessments if given. The objective of the FICA tool was to demonstrate spiritual screening in the literature.
Survey and Interview Questions
The following questions were created to help identify gaps and gain as to why spirituality has been neglected or avoided by some therapists.
-
How do you assess a patient’s spiritual needs?
-
Can you tailor to a patient’s spiritual needs/problems in consultation with the patient?
-
Can you write a report on a patient’s spiritual functioning?
-
Who do you refer him/her to for spiritual care?
-
Why is it important for a therapist to ask about spirituality?
-
How is spiritual well-being defined?
-
Why has spirituality been neglected or avoided by some therapists?
-
How can spirituality be encouraged in therapy?
-
How do patients respond to your spiritual care assessments?
-
How have you collaborated with clergy or local chaplains?
Spiritual Screening
Data Collection and Analysis
Data was gathered from the online Survey Monkey and phone interviews. Participants completed a five-question online survey and answered five questions during phone interviews. The study consisted of eight themes. The online survey was helpful in gathering the quantitative data on participants responses. It provided a great analysis of participants’ understanding of faith and religion regarding spiritual care. The PI interviewed participants and took notes of their responses. The participants were able to demonstrate if they were trained in assessing their patients in spiritual care by giving examples of how they assess patients.
Findings of the Study
Results
Eight themes emerged to develop study findings. The eight themes were developed from both the online survey and interviews using a thematic analysis process.
-
Clinicians and chaplains agreed it is important to ask clients about their spiritual background.
-
Clinicians and chaplains agreed spiritual well-being is defined as faith, values, and beliefs.
-
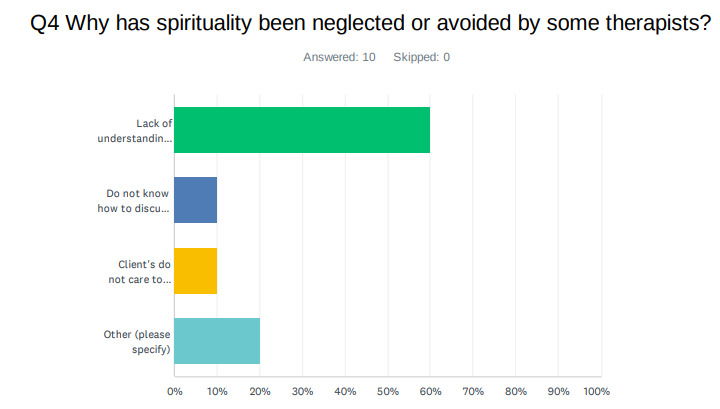
Clinicians and chaplains agreed that lack of understanding has resulted in spirituality being neglected or avoided by some therapists.
-
Chaplains and clinicians agreed that more education and training is needed to encourage spirituality in therapy.
-
Most participants agreed clients enjoy their spiritual care assessments.
-
Chaplains and clinicians use spiritual assessment tools.
-
Clinicians agreed to make referrals to local chaplains and clergy.
-
Chaplains and clinicians agree to collaborate to assist their patients with spiritual care and mental health.
Theme 1. Why is it important for a therapist to ask about spirituality?
Eight participants shared they feel comfortable assessing their client’s spiritual background. One chaplain spoke about the importance of building a rapport and tried to find meaning behind the mental health diagnosis. “It is important to engage patients when they first come in and develop a rapport and assess if they have an active faith background.” The participant believed that assessing faith background would help with the mental health diagnosis. On the survey, three of the ten (30%) participants responded it is important for a therapist to ask about spirituality to find out client’s faith background; two of ten (20%) participants stated to connect with client and build rapport; two of ten (20%) participants stated to help with treatment plan, and three of ten (30%) participants selected others to provide their own answer. For example, one participant believed it is important to address the whole person rather than the part of a person for better health outcomes. A clinician also believed asking about their client’s spirituality will uncover root causes for physical/psychological symptoms, “Thus, asking about spirituality helps the therapist find out the client’s background, connect with the client, build rapport, and help with the treatment plan.”
Theme 2. Definition of spiritual well-being
There was an equal share of clinicians and chaplains agreeing that the definition of spiritual well-being is, above all: discovering meaning and purpose, peace of mind, faith, values, and beliefs. One participant stated, “Spiritual well-being can include all the above: discovering meaning and purpose in life, peace of mind, plus faith, values and beliefs.” According to the results from chaplain and clinician online survey, three of ten (30%) participants responded discovering meaning and purpose in life, one of ten (10%) participants selected peace of mind, three of ten (30%) participated chose faith, values, and beliefs, three of ten (30%) participants provided their own answer.
Theme 3. Spirituality is neglected or avoided by some therapists
Results showed six of ten (60%) participants agreed that spirituality has been avoided and neglected due to lack of understanding of spirituality and religion with one participant noting, “Clinicians are not pastors, ministers, or priest.” Additionally, one participant selected they do not know how to discuss spirituality and religion, one participant selected client’s do not care to discuss, and 20% of participants provided their own response, with one participant sharing, “I think it depends on therapist’s personal philosophy of administering therapeutic practice.”
Theme 4. How can spirituality be encouraged in therapy?
Six of ten (60%) participants felt more education and training are needed in spiritual care to be integrated within therapy. For example, “By engaging clinical pastoral practitioners who have an in depth understanding of the spiritual care.” Another participant stated there needs to be, “More education and training for clinicians on the impact of spirituality on health, plus more collaboration with local clergy.” One therapist suggested clinicians should focus on their own spiritual growth.
Theme 5. How do clients respond to your spiritual care assessments?
Six of ten (60%) participants agreed clients enjoyed their spiritual care assessment. One participant stated most clients desire for therapist to integrate spiritual care within treatment. “Most of the time clients desire the therapist to integrate spiritual care within treatment. I see clients may not enjoy spiritual care assessment questions, but they find it beneficial to reflect on these personal growth questions.” Four out of five (20%) chaplains mentioned the importance of developing a rapport with patients and assessing their faith background to assess their spiritual needs.
Theme 6. How do you assess a patient’s spiritual needs?
Two out of ten (20%) chaplains and clinicians use existing spiritual assessment tools to gather spiritual backgrounds. Others use their own intake assessments to assess spiritual care by taking notes for treatment plans. According to the results of the phone interview, two out of five clinicians provided the assessment tools they use for spiritual care. One clinician (participant number 4) stated they use Dr. Peter Scazzero’s Emotional Healthy Discipleship Personal Assessment and the U.S. Army’s Spiritual Fitness Inventory tools. They shared that the Emotional Health Discipleship Personal Assessment is based on bible verses and emphasizes seven marks of emotionally healthy discipleship. According to clinicians, patients learn whether they are in the emotional infant, child, adolescent, or adult stage for each of the seven marks.
For reporting of patients spiritual functioning, one clinician (participant number 5) stated they record weekly clinical progress in Detailed Assessment of Posttraumatic Stress (DAP) and in the Subjective, Objective, Assessment and Plan (SOAP).
Theme 7. Who do you refer to for spiritual care?
Three out of five (60%) clinicians stated they refer clients to local pastors and clergy. One clinician stated, “In the midst of counseling, I may refer patients to faith-based quality resources for greater self-improvement. I will refer patients to pastors or trained spiritual advisors who understand the multi-dimensional person-that we are many parts, but all one body.” The study found therapists often refer their clients to a local church, spiritual advisor, and local pastors. A hospital chaplain mentioned it is a challenge collaborating sometimes with other clergy because they are not familiar with a mental health environment. They also stated it can be a challenge to find various bibles or resources for different faith backgrounds.
Theme 8. Collaborations with local pastors and clergy
Both chaplain and clinicians collaborate to meet the patient’s spiritual needs. One clinician stated, “I often ask clergy and spiritual directors how best to pray for clients whether on-the-ground with patients or from afar.” A chaplain stated many of the local clergy that visit the state hospital are not trained in mental health. They sometimes are not comfortable in the mental health setting.
The findings support that integrating spiritual care within mental health can improve treatment options and spiritual public health and that use of validated tools such as the FICA may help address gaps of under addressed spiritual needs of patients.
In the literature review, Fruehwirth, Lyer and Zhang (2016) suggested clinicians and psychologists struggle with integrating religion within their mental health treatments because of a lack of understanding (Fruehwirth et al., 2016). Six of ten (60%) of participants felt clinicians do not assess spiritual care because of lack of understanding and close to 20% shared they do not know how to discuss spiritual care to their patients. This result is very similar to the human services integrating spiritual care within social work. According to Regis (2025), social workers do not feel prepared to initiate spiritual discussions due to lack of training.
Discussion
The literature focused on four overarching questions: 1) How can integrating spiritual care improve mental health with proper treatment and spiritual public health? 2) Do mental health clinicians use spiritual care assessments and are they trained in spiritual care, and if so, how? 3) Do mental health clinicians collaborate with clergy, and if so, how? 4) What barriers do mental health clinicians face in integrating spiritual tools into mental health treatment? This study examined the gap that occurs when clinicians lack knowledge and education to provide spiritual assessment and care to patients. In addition, it examined if clinicians collaborate with chaplains to assist patients with their spiritual needs.
Eight themes emerged to develop study findings. 1) Why is it important for a therapist to ask about spirituality? 2) Definition of spiritual well-being. 3) Spirituality is neglected or avoided by some therapists. 4) How can spirituality be encouraged in therapy? 5) How do clients respond to your spiritual care assessments? 6) How do you assess a patient’s spiritual needs? 7) Who do you refer to for spiritual care? 8) Collaboration with local pastors and clergy.
The review of literature found clinicians should have more discussions and lectures on religion and spirituality. More clinical spiritual assessments need to be conducted during mental health visits and for spiritual public health. Lastly, there needs to be more collaborations with the clergy community and clinicians.
The findings indicate integrating spiritual care within mental health may improve and be a treatment option for patients and spiritual public health. The literature review mentioned spirituality is considered a social determinant of health and integrating spiritual factors into public can bring good outcomes. The results showed six of ten (60%) of participants believe spirituality has been neglected or avoided by some therapists due to lack of understanding.
Recommendations
One recommended solution for clinicians and practitioners is to be open to spiritual care assessments because it will allow communications to open to learn about a patient’s values and beliefs. It will lead to a better understanding of their faith background and to find if there are positive or negative coping skills. Also, a spiritual assessment can facilitate the creation of a spiritual care plan that will help patients achieve wholeness and a greater sense of peace and well-being. The findings also suggest that more education and training for clinicians and staff is needed to prepare themselves in providing spiritual care to their patients to screen for spiritual concerns.
Clinicians should have more discussions and lectures on religion and spirituality during their graduate-level courses. Mental health providers will feel more comfortable with referring patients to clergy and conducting spiritual assessments once they have had proper training and education. Spiritual care integration can change lives and bring about lifestyle transformation. Evidence-based research in spiritual care can give insight to what chaplains can provide for patients to bring about a better quality of life.
Recommendations for future studies or scholars who desire to study spiritual care would be to continue to dig deep into the research of integrating spiritual care within mental health. It is an important component of spiritual health. Also, more research is needed on the importance of spiritual interventions to clinicians and chaplains about spiritual counseling, meaning-focused meditation, or psychotherapy. Lastly, an important follow-up study would be to find ways to strengthen the utilization of spiritual assessment tools rather than just an intake assessment on spiritual care.
Limitations
The study consisted of chaplains and clinicians who were therapists. Therefore, the limitations included not having other professional healthcare workers such as nurses and physicians to share their experience in spiritual care. Sometimes scheduling was difficult due to participants living in various states such as Arkansas, Georgia, Tennessee, Texas, Alabama, and Utah. However, participants were very pleasant and easy to work with. The PI was able to obtain the data for the study.
The study’s results are aligned with prior studies and support indicates spiritual care can provide hope and motivation and improve spiritual public health. Therefore, integrating spiritual care may improve mental health treatment within the mental health industry. In doing so, clinicians must learn and request more spiritual resources or definitions. Clinical spiritual assessments should be integrated into the care of patients with mental health conditions. More collaborations with the clergy community and clinicians are needed. In addition, improved clinical training on religion and spirituality is needed.
Conclusion
Overall, the study’s conclusions demonstrate the importance of integrating spiritual care within mental health and spiritual public health. Spiritual care can bring meaning, purpose and better outcomes for public health. The reviewed literature found reimagining the future of public health should address integrating deeply valued spiritual determinants of health that also shape ultimate meaning, purpose, transcendence, and connectedness for individual well-being and population health (Long, Symons, et al., 2024).
The findings of this study showed the overall spiritual needs of patients may be unaddressed if validated tools such as FICA are not being used by clinicians or chaplains. Spiritual assessment tools, can enhance whole-person care by identifying which patient might benefit from spiritual support or spiritual community participation (Long, Symons, et al., 2024). Current and future studies into these areas will help transform integrating spiritual care within mental health and spiritual public health.